For Dental Payers:
SmartClaimFocus™
An AI-Powered Platform to Optimize the Utilization Management Process
Fluent™, a leading provider of AI-powered oral health analytics, introduces SmartClaimFocus™, a new platform designed to help payers optimize utilization management, identify fraud, waste, and abuse (FWA), and strengthen adjudication strategies.
SmartClaimFocusTM
An AI-Powered Solution to Optimize the Utilization Management Process
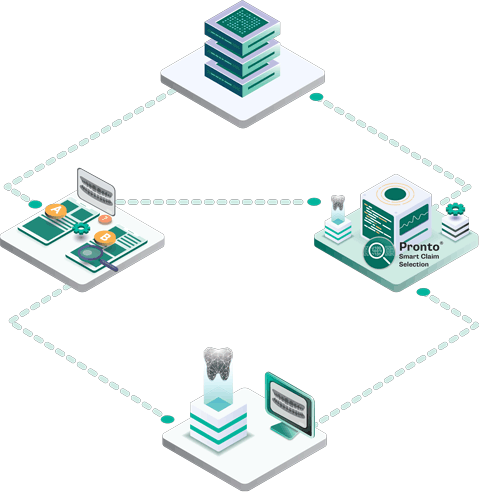
Designed for payers seeking a lighter technology lift, SmartClaimFocus™ is a streamlined SaaS platform that performs sophisticated retrospective reviews to uncover suspicious provider behavior.
Leveraging a powerful rules-based pattern recognition engine, it analyzes post-payment data to highlight specific providers and procedural areas that are most likely to benefit from a focused audit.
This targeted approach allows you to bypass the noise and deploy your resources where they will have the greatest impact, ensuring a more strategic and cost-effective utilization review process.
Why SmartClaimFocusTM is Different
Deep Data
SmartClaimFocus™ combines dental claims data from DentaBase® —the largest multi-payer dental claims database with Fluent’s AI-powered, algorithm-driven rules engine.
Analytics
By analyzing your claims history against practice pattern benchmarks, it identifies statistically significant outliers and highlights areas where targeted review will have the greatest impact.
Intelligence
This intelligence empowers you to direct resources where they will yield the biggest return, cutting unnecessary costs and driving smarter, data-backed decision-making.
Cost-Effective Utilization
This targeted approach allows you to bypass the noise and deploy your resources where they will have the greatest impact, ensuring a more strategic and cost-effective utilization review process.
Fluent in smart claim selection
SmartClaimFocus™ at a Glance:
- Provider-Level Breakdown: Drill down within each procedure rule to see which specific providers are most frequently flagged for potential outlier behavior, enabling a targeted approach to reviews.
- Rule Prioritization: Rules are ranked by FWA potential incremental savings, allowing users to focus on the highest-impact opportunities first.
- Focused Review: Pinpoint high-impact risk areas and select specific providers and CDT codes for targeted review. You can also monitor review volume realized and estimated savings directly within the platform.
- Processor View: See where adjudication processes are intercepting standard FWA processing rules, along with the financial impact. This provides granular insight into the effectiveness of specific rules.
- Data Export: All views support data export, making it easy for teams to share information and coordinate follow-up actions.
- FWA Impact: Estimate the potential financial impact tied to inactive rules to identify opportunities for increased efficiency and cost savings.
LEARN MORE
Contact Us
End-to-end efficient utilization review optimization in a single, technology-enabled clinical decision support tool. SmartClaimFocusTM can help your team maximize review effectiveness and enhance your ROI.

