For Dental Payers:
SmartClaim™ Solutions Suite:
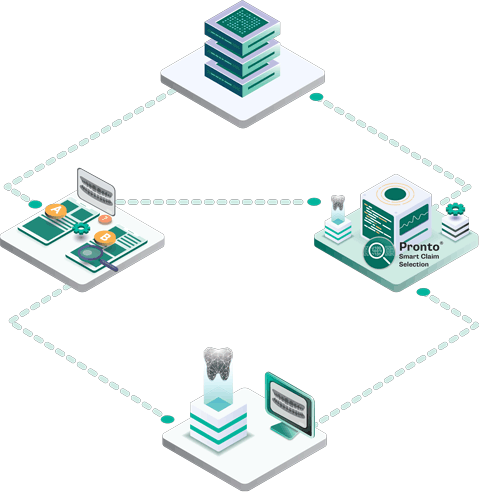
The Suite Delivers Data-Driven, Cost-Efficient Utilization Review
Fluent™, the leader in oral health analytics, today introduced the SmartClaim™ Solutions Suite, designed to modernize utilization review with a more strategic, cost-efficient approach.
Rather than directing all utilization review eligible claims to either dental consultants and/or or standalone AI image analysis, SmartClaim™ Solutions Suite takes a strategic approach based on payer-specific resources, objectives, and philosophy.
The goal is to meet payers where they are by offering flexible, proven solutions. By targeting only the claims that truly warrant deeper scrutiny, this suite helps your team identify fraud, waste, and abuse (FWA) while significantly strengthening network relationships.


Finally, cost-effective UR solutions that meet the needs of any payer regardless of size, resources, or philosophy.
SmartClaimTM Solutions Suite consists of:
SmartClaimSelect™ (Targeted Adjudication)
- What it is: A deep data integration that rank-orders risk in real-time.
- The Benefit: Auto-adjudicate low-risk claims and reserve expensive AI image reviews only for high-risk outliers.
SmartClaimFocus™ (Retrospective Review)
- What it is: A lightweight SaaS platform for retrospective analysis.
- The Benefit: Identify suspicious provider behavior patterns and deploy your audit resources where they have the greatest impact.
With SmartClaim™ Solutions Suite,
Payers address FWA detection in a cost-efficient manner:
Fewer backlogs
Happier providers
Smarter allocation
of review resources
Higher ROI
LEARN MORE
Contact Us
End-to-end efficient utilization review optimization in a single, technology-enabled clinical decision support tool. SmartClaimTM Solutions Suite can help your team maximize review effectiveness and enhance your ROI.
